Common Employee Benefits Confusion and How HR Can Clear It Up
Why Employees Don’t Understand Their Benefits
Employee benefits packages are often layered with jargon, multiple plan options and confusion for which plans they and their dependents are enrolled in that can be difficult for employees to navigate. Even with open enrollment meetings and benefit summaries, many employees remain unclear on what their plans actually cover or how to use them effectively. These challenges are common and reflect the inherent complexity of benefits—not shortcomings in HR teams.
Common Misconceptions Employees Have
Census data is essential for securing accurate bids from providers. Whether you're considering a level-funded plan, joining a PEO, or managing a large group policy, detailed census data can make or break your benefits strategy.
Deductibles vs. Out-of-Pocket Maximum:
Many employees assume that once they meet their deductible, they won't have to pay anything else. In reality, the out-of-pocket maximum includes the deductible, plus any copays and coinsurance, up to a certain limit. Misunderstanding this distinction can lead to unexpected costs.
In-Network vs. Out-of-Network:
Employees often believe they can see any provider and receive the same coverage. However, using out-of-network providers usually results in higher costs and limited coverage. Additionally, sometimes employees will ask if a provider accepts their coverage, instead of if they are in-network. A provider might accept their insurance, but be out of network. Clarifying this early can prevent costly surprises.
Copays versus Coinsurance:
These two cost-sharing mechanisms are frequently confused. Copays are fixed amounts for specific services, while coinsurance is a percentage of the service cost. Not knowing the difference can affect how employees budget for healthcare expenses.
Plan Types (HMO, PPO, HDHP):
Understanding the limitations and benefits of each plan type is critical. HMOs typically require referrals and network restrictions (such as no out-of-network), PPOs offer more flexibility, and HDHPs have higher deductibles but allow HSA contributions. Employees often select plans without fully grasping how they align with their needs.
Common types of plans include:
- Health Maintenance Organization (HMO): Requires members to use a network of doctors and get referrals from a primary care physician.
- Preferred Provider Organization (PPO): Offers more flexibility in choosing providers and does not require referrals.
- High Deductible Health Plan (HDHP): Comes with higher deductibles and eligibility for a Health Savings Account (HSA) and can be paired with a PPO or HMO plan.
- Exclusive Provider Organization (EPO): Similar to an HMO but does not require referrals, while still restricting care to in-network providers only.
- Point of Service (POS): Combines features of HMO and PPO plans, requiring referrals for specialists but allowing some out-of-network coverage.
AEIS assists HR teams by evaluating plan designs, educating employees on the trade-offs between options, and aligning offerings with the unique demographics of each workforce. We support a broad range of coverage areas including medical, dental, vision, life, and disability insurance. Our support includes custom comparisons, one-on-one consultations, and guidance to help ensure employees make informed choices that fit their healthcare needs and financial situations.
Lack of Clarity in Communications
Overwhelming Information
Benefits communications frequently include dense legal language, numerous acronyms, and overly technical explanations. Without proper context or simplification, employees may skim through materials without fully understanding them.
Infrequent Communication:
Benefits are typically discussed during onboarding or open enrollment, and then seldom revisited. This leaves employees with limited opportunities to revisit information or ask questions as their life circumstances change
Lack of Personalization:
Benefits communications often adopt a one-size-fits-all approach. Employees with different needs, such as a single young adult versus a parent with dependents may find it hard to determine which options suit them best without personalized guidance.
The Hidden Costs of Benefits Confusion
When employees don’t fully understand their benefits, the impact extends beyond individual frustration. Employers can face a range of hidden costs that affect the organization as a whole.
1.
Underutilization of Benefits: If employees don’t know how to access or maximize their benefits, they may delay medical care, miss out on preventive services, or skip financial wellness tools—all of which can lead to higher claims costs or increased absenteeism.
2.
Increased Administrative Burden: Confused employees are more likely to reach out to HR with repetitive questions or require extra time during enrollment periods. This adds strain to already busy HR teams.
3.
Reduced Employee Satisfaction and Retention: Benefits play a significant role in job satisfaction. If employees feel uncertain or misinformed about what they’re offered, it can diminish trust in the employer and increase turnover rates. Studies have shown employees are more likely to value their benefits when they understand them, even if the benefits are modest, than when generous benefits are poorly understood.
4.
Compliance Risks: Miscommunication or lack of clarity around required notices, eligibility windows, or coverage details can inadvertently lead to non-compliance with state or federal regulations, particularly in California where rules frequently evolve. Fines from these kinds of oversights can be incredibly costly to employers.
Effective Strategies for HR to Improve Communication
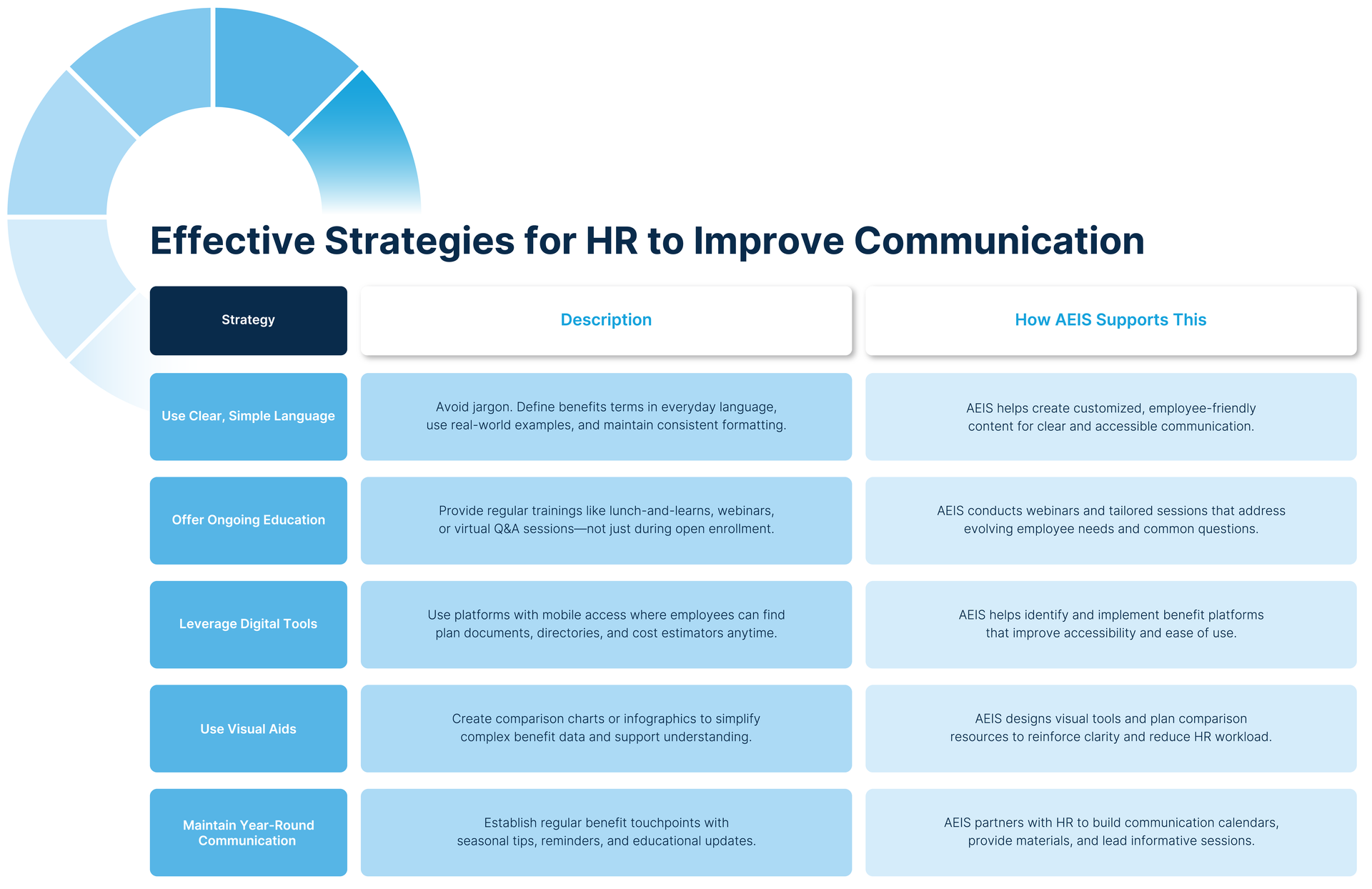
Click here to download the Effective Strategies for HR graphic.
Use Clear, Simple Language in Benefit Communications
Avoid jargon and use straightforward language to explain benefits concepts. Define terms plainly and offer real-world examples. Consider rewriting summaries with employee-friendly terminology and using consistent formatting across materials. AEIS supports HR teams with clear, customized content that helps make benefits communication more accessible and effective.
Offer Regular Training and Benefit Walkthroughs
Don’t wait for open enrollment. Provide ongoing education through workshops, lunch-and-learns, or virtual Q&A sessions. Interactive sessions allow employees to ask questions and gain clarity, especially as their needs evolve. AEIS can support these efforts by conducting webinars and personalized sessions that address common concerns.
Leverage Digital Tools or Benefit Platforms for Easy Access
Invest in user-friendly benefits platforms where employees can easily access plan documents, provider directories, and cost estimators. Mobile access and 24/7 availability empower employees to get the answers they need when they need them. As your partner, AEIS can help identify and integrate digital solutions that align with your team's goals.
Provide Visual Aids like Charts or Comparison Tables
Help employees compare plan features, costs, and coverage levels with visuals that break down complex data. Simple comparison tables and infographics can dramatically enhance understanding and reduce reliance on HR for explanations. AEIS provides tailored visuals and communication aids that reinforce employee comprehension.
Create a Year-Round Communication Plan
Move beyond a once-a-year push. Develop a calendar of touchpoints to regularly share reminders, seasonal tips, and educational content. This ongoing approach reinforces understanding and helps employees feel supported throughout the year.
An essential part of this strategy is leveraging your benefits broker. A broker can assist in developing a structured communication calendar, provide ready-to-use materials, and lead educational sessions. At
AEIS, we work alongside HR teams to bridge the benefits communication gap, helping to ensure that employees not only understand their options but feel empowered to use them. Our collaborative approach lightens HR's administrative load while strengthening employee engagement.
Clarity around
employee benefits is not a one-time task. It is an ongoing responsibility that directly affects organizational health, employee morale, and compliance.
Disclaimer: Any information related to compliance, laws and regulations, or other subject matters in this blog is intended to be informational and does not constitute legal advice regarding any specific situation. The content of this blog is based on the most up-to-date information that was available on the date it was published and could be subject to change. Should you require further assistance or legal advice, please consult a licensed attorney.



